7 Examples of AI in Healthcare: Our Digest of What Works in the Industry

Finney Koshy
Product Owner
Share to AI
Ask AI to summarize and analyze this article. Click any AI platform below to open with a pre-filled prompt.
Artificial intelligence is revolutionizing healthcare delivery and patient outcomes across multiple domains. Instead of wading through abstract predictions or academic theory, you actually need concrete examples of AI in healthcare and how hospitals, clinics, and health tech leaders are actually using AI to improve patient outcomes, reduce costs, and streamline operations.
At Aloa, we build healthcare AI that achieves those common goals. HIPAA-safe data pipelines? Check. EHR integrations that don’t torch your workflows? Absolutely. Tools your clinicians won’t curse at? That’s the bar. We’ve worked alongside leaders like you to take AI from “cool pilot” to “part of daily rounds.”
So here’s what we’re serving up: real-world use cases that answer how AI is helpful in healthcare, such as:
- Diagnostic imaging to improve accuracy
- Medical image analysis for more reliable detection
- Predictive analytics to flag risk earlier
Whether you’re a healthcare professional or tech leader, this article helps you quickly identify what’s working now so you can apply those lessons to your own strategy. We’ll show you why these examples of AI in healthcare are worth looking at and how you can implement something similar.
1. AI-Powered Diagnostic Imaging: Revolutionizing Medical Image Analysis
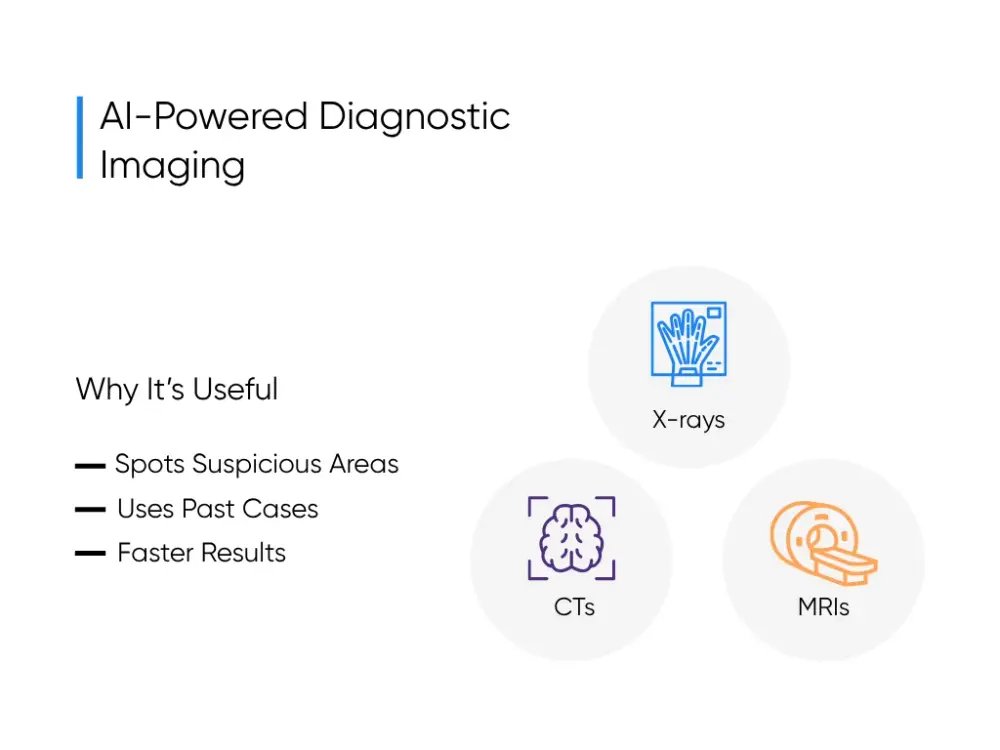
AI in diagnostic imaging refers to software that reads scans (X-rays, CTs, MRIs) alongside the radiologist. It highlights suspicious spots, compares them against thousands of past cases, and speeds up reporting. As one of the clearest examples of AI in healthcare, it turns hours of image review into minutes, with better accuracy.
Radiologists go through hundreds of scans a day, each with slice after slice to review. It’s no surprise things slip when the list never ends (we’d miss a detail or two ourselves). AI picks up that slack, running pattern-spotting algorithms on millions of images labeled by human experts. They flag what’s easy to overlook and push urgent scans to the top.
And the numbers back it up. In breast cancer screening, AI support has improved detection rates and reduced false negatives, so patients get treated earlier when odds are highest. Aidoc also showed a 61% drop in turnaround time for brain bleed scans. That means faster care, fewer repeat scans, and radiologists with more time to focus on the toughest reads.
The winners start small, validate locally, run bias checks, and make it so seamless the tech fades into the background. That’s when the use of AI in healthcare stops being a shiny demo and becomes the extra resident you actually trust.
2. Medical Image Analysis: AI-Powered Disease Detection
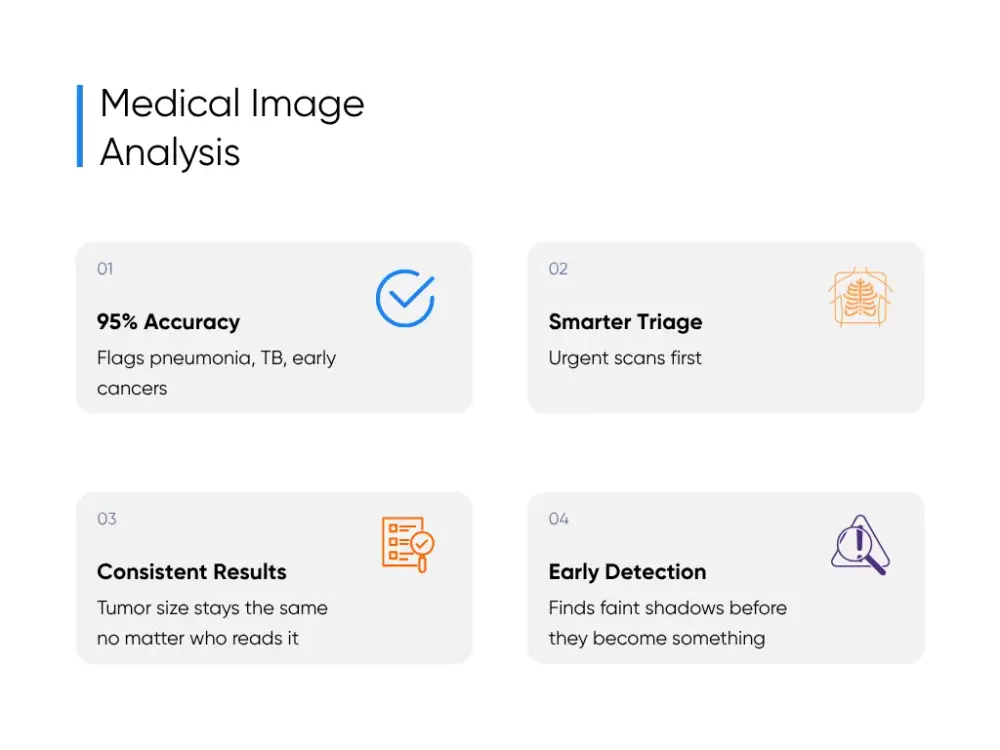
If diagnostic imaging is the equivalent of showing you an obvious crash that took place on the highway, image analysis is the equivalent of pointing out a tiny crack in the windshield you didn’t even notice.
It does it by prioritizing urgent scans so the critical cases get read first, but also having the capacity to spot things that aren’t related to the critical issues that doctors are usually focused on. Deep learning can process every scan that you feed into it and start recognizing patterns. All of that becomes valuable analysis that doctors can have access to the moment they need to.
Right now, chest X-rays are being read at 95% accuracy, flagging pneumonia, TB, and early lung cancers before patients are discharged. Pre-screening tools cut CT wait times in half by moving trauma scans to the front. Tumor measurements stay consistent no matter who’s reading them (Alice, Bob, or the algorithm). And faint shadows that used to slip by are now flagged at stage 1 instead of stage 3.
And that’s the part we geek out on at Aloa. With our machine learning services, we help train models on real hospital data and tune them so they actually work in the field. And the trick is sliding the tech into clinical workflows so smoothly it just feels like the system got smarter.
3. Predictive Analytics for Patient Risk Assessment
Predictive analytics is basically the healthcare version of checking your weather app. Only instead of “grab an umbrella,” it’s “this patient could crash with sepsis.” Not a crystal ball. Not sci-fi. Just practical AI capabilities and your data stitched together.
Here’s the idea in plain English. AI chews on health data: electronic health records, lab results, vital signs, old admissions, even the lifestyle notes tucked away at the bottom of the chart. It doesn’t hand you a guarantee. It taps you on the shoulder and says, “Hey, this one’s trending risky.” It’s the kind of nudge that can turn a close call into a non-event.
At Cleveland Clinic, predictive analytics powered a readmission risk score that pulled in both clinical data and social factors like housing and support networks. It flagged the patients most likely to come back within 30 days, giving the team a chance to line up follow-ups and extra help before the next ER visit. That cut readmissions by about 10%, meaning fewer patients cycling through the same bed and fewer staff groans of “not you again.”
The real kicker? It flips the script. Healthcare usually plays defense (react fast when the crisis explodes). Predictive analytics lets you play offense. You catch sepsis before it spirals. You keep patients out of the revolving hospital door. And for once, it feels like you’re steering the ship instead of frantically bailing water.
4. AI-Powered Drug Discovery: Accelerating Pharmaceutical Development
If you’ve ever watched how long it takes to get a new drug to market, you know that it’s a lengthy process.
AI can make an impact during this manual drug discovery process. Machine learning models can sift through millions of molecules at speeds no human team could dream of. A recent review showed AI-enhanced screens consistently outperform traditional wet lab runs when it comes to finding promising hits. What used to take years now takes days.
And COVID-19 proved the concept. During the pandemic, medical research teams leaned hard on AI. Pfizer used machine learning to clean massive clinical trial datasets in just 22 hours, a job that usually takes over a month. That shaved weeks off decision timelines when every day counted.
Although drug discovery will remain a detailed process, AI can play a role in helping labs create promising drugs with fewer resource-related bottlenecks.
5. Clinical Decision Support Systems: AI-Enhanced Treatment Planning
A Clinical Decision Support System (CDSS) is basically the extra set of eyes you wish you had on a hectic shift. It lives in the EHR, skimming labs, allergies, and protocols in real time, then drops you a quiet nudge when something looks risky. Less “gotcha exam,” more “hey, maybe rethink that before it backfires.”
In practice, that means CDSS pulls from research and patient data to suggest personalized treatment plans, flashes safety alerts when a drug and lab result don’t mix, and does it all without forcing extra logins or clicks. The best part? Hospitals using it the right way have cut medication and diagnostic errors by 53%. That translates to fewer complications, smoother discharges, and more time on actual patient care instead of paperwork.
Picture it: you order ceftriaxone. CDSS clocks the allergy note, notices the kidney function, and steers you toward a safer option. You adjust the order. The patient avoids a setback. The hospital avoids a bounce-back admission. And you get to play it cool, knowing your digital safety net had your back, even if it was just a line of code baked into the EHR.
6. AI in Medical Training and Education: Enhanced Learning Systems

AI can transform medical training in a few ways:
- Virtual reality surgical simulators: Think of this as flight school for surgeons. A headset and haptic tools for surgical procedures can be highly effective.
- Adaptive learning content: The general principle of creating adaptive learning experiences also applies to AI in healthcare. Interactive content that provides timely feedback can help clinicians improve more quickly and gain greater confidence.
- Digital patient scenarios: Generative AI can spin up patients with rare diseases, tricky complications, or other curveballs.
That’s also why we built Aloa as a research and education hub. We publish guides, case studies, and lessons learned so healthcare teams and health tech leaders can keep leveling up right alongside the tools they’re adopting. As builders at heart, we sketched out how we pieced together the engine that powers medical transcription (with speech recognition) in practice.
7. Remote Patient Monitoring: AI-Powered Home Healthcare
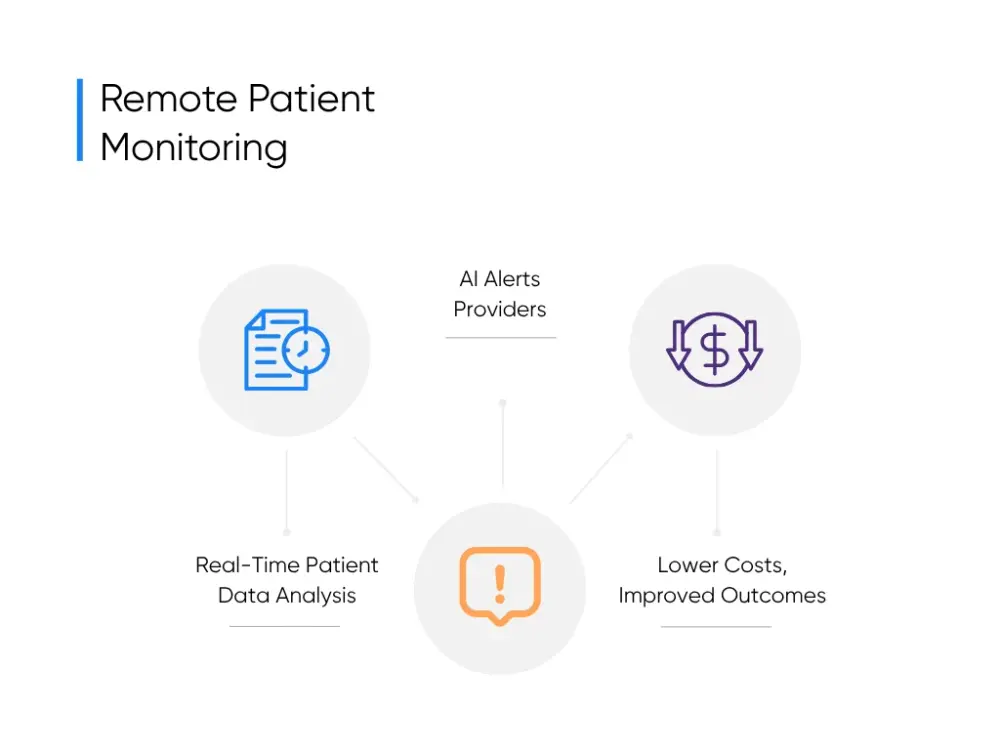
Remote Patient Monitoring (RPM) is healthcare that doesn’t clock out when the patient leaves. Picture a watch, a cuff, or a glucose patch streaming heart rate, oxygen, and blood pressure nonstop. AI is the one glued to the feed, catching the subtle shifts humans would probably miss after their third double shift. When a reading drifts, it pings the care team before a “small blip” becomes a “big problem.”
Here’s how hospitals are already putting it to work:
- Diabetes Management: Continuous glucose monitors paired with AI track blood sugar around the clock, spot spikes, and send nudges that prevent swings from turning into ER visits.
- Post-Surgery recovery: RPM systems stream vitals from home, and AI flags early shifts so doctors adjust care before a small complication becomes a readmission.
- Senior Care at Home: Wearables log movement, meds, and daily activity. AI taps a caregiver when irregularities show up, keeping more older adults safe at home and out of preventable ambulance rides.
So instead of waiting for trouble to roll back in, providers see it coming and head it off. Sure, the percentages bounce around depending on the study, but the pattern holds: fewer emergencies, lower costs, and a whole lot less stress on everyone.
Key Takeaways
The healthcare industry is seeing the best examples of AI in healthcare happen now. They’re trimming readmissions, flagging risks, improving patient outcomes, and giving healthcare providers room to breathe. The leaders making it work don’t wait for “perfect.” They pick one problem, try AI alongside what they already do, and double down when it delivers.
If you’re experimenting with AI or just staring at a blank page wondering where to start, let’s talk. Aloa builds AI that fits into the grind of real hospital life. Not “science fair” prototypes. Not dashboards nobody logs into. Tools that live where your staff already works, so adoption feels less like a revolt and more like… Tuesday.
And we’d love to hear what’s tripping you up right now. Drop your biggest challenge in our AI Builder Community on Discord. Lurker mode more your thing? Our Byte-Sized newsletter is quick, real, and mercifully jargon-free.
AI in healthcare is moving fast. The fun part? You don’t have to figure it out alone. We’re building this future together.
FAQs About AI in Healthcare Examples
What are the main benefits of AI in healthcare today?
Honestly, the biggest win is time. AI takes the boring, click-click paperwork off your plate so you can actually focus on people, not screens. It spots issues faster, trims hours of administrative tasks, and cuts costs across healthcare applications along the way. Want proof beyond our rambling? Our breakdown of AI applications in healthcare highlights three real benefits already landing in 2025.
Are these examples of AI in healthcare accessible to smaller healthcare organizations?
You don’t need a billionaire’s budget or a campus the size of a football stadium. A lot of AI technologies are cloud-based now, which makes them surprisingly doable for smaller clinics. Diagnostic imaging, telemedicine, even decision support often land in the $50,000–200,000 range a year. Surgical robots? Still in the “Ferrari” category. But the good news is that it’s getting cheaper and more accessible every year.
Can AI in healthcare be safe and compliant with regulations?
Short answer: yes. Longer answer: yes, but only if you do your homework. HIPAA, FDA approval, audits for bias, data privacy, and data security. Skip those and you’re asking for trouble. We’ve spelled out the practical safeguards in our guide on making AI models HIPAA-compliant. It’s not flashy, but it’s the stuff that keeps lawyers from sweating through their suits.
What common implementation mistakes should healthcare organizations avoid?
Oh, the classics. Buying AI without a clear business case. Forgetting your IT folks are already drowning in projects. Skipping staff training and hoping the system magically works. Or our favorite: expecting it to deliver miracles on day one. AI isn’t instant ramen. It needs setup, support, and some patience before it starts paying off.
How do healthcare organizations measure success for these AI implementations?
Please don’t just pat yourselves on the back for “having AI.” That’s not a metric. Track what matters:
- Clinical outcomes: More accurate disease diagnoses, safer patients, better treatments.
- Operations: Faster processes, smoother workflows, less staff burnout.
- Financials: Cost savings, ROI, even fresh revenue.
- Satisfaction: Healthcare professionals who actually use it, and patients who notice the difference.
The smart teams set a baseline before rollout, then measure over 12–24 months. That way, you know if your AI is a lifesaver… or just another dashboard collecting dust (and we’ve all got enough of those already).